Why Nuance is Not the Enemy
I was blocked by a science page for discussing vaccine schedules. It convinced me we need a better place to talk.
This Article is part of the Trust Project: Rebuilding Trust in Health Messaging with Radical Honesty.
When Clinical Nuance meets Ideology
A few days ago, I was blocked by a large "pro-science" page on social media. My transgression wasn't spreading misinformation or being abusive. It was for attempting to have a nuanced conversation about the routine newborn vaccination schedule.
The exchange was frustrating, but ultimately clarifying. It showed me in sharp relief that the algorithms and engagement-driven nature of social media are fundamentally hostile to the kind of conversations that doctors and parents have every single day. The platforms reward absolutism and punish nuance. They are built for declaring, not discussing.
This Substack is the antidote to that. This is the beginning of a space where we can explore the complex, messy, and deeply human realities of medicine without fear of being shouted down or silenced.
The Spark: A Paediatrician's Dilemma
The topic that got me blocked was the newborn Hepatitis B (HepB) vaccine.
In medicine, few things are more rigorously tested and proven than the benefit of vaccines. The immunisation schedule is one of the greatest public health triumphs in human history. I advocate for it passionately. But effective advocacy requires trust, and trust requires conversation.
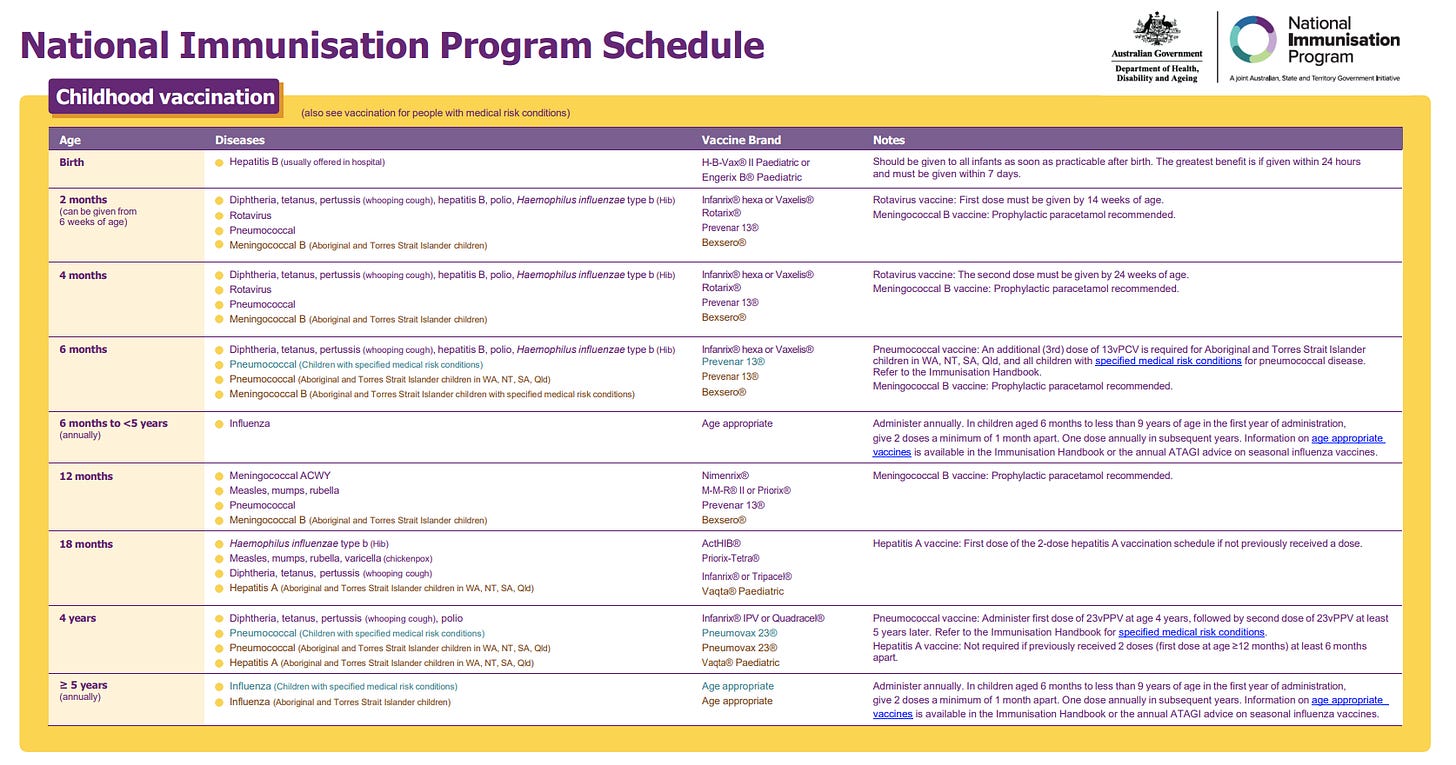
Source: Adapted from the Australian National Immunisation Program Schedule.
Note: This schedule is current as of July 2025. Please consult the official source for the most up-to-date information.
Here was the clinical scenario I tried to discuss:
In a country like Australia, the routine schedule recommends a birth dose of the HepB vaccine for all infants. However, in other developed countries, like New Zealand (where I trained), the approach is different. There, the birth dose is targeted specifically at infants at high risk of transmission - primarily those whose mothers are HepB positive. For low-risk infants (where the mother has been screened and is negative), the HepB vaccine course starts at 6 weeks.
Source: The Immunisation Advisory Centre (IMAC), New Zealand.
Note: This schedule is current as of July 2025. Please consult the official source for the most up-to-date information.
Why the difference? A rigorous risk-benefit analysis.
For a low-risk infant, the birth dose adds minimal additional long-term protection compared to starting the immunisation course at 6 weeks. The argument for it is that it closes a theoretical, tiny window of risk.
The argument against it, and for the targeted approach, is also compelling. It's one less intervention in the first few hours of life for a low-risk baby, reducing it from 4 shots to 3 for the same long-term immunity outcome. In my clinical experience, this matters. New parents are often anxious. My job is to maximise the protection for their child, and sometimes that means making a strategic compromise to maintain the therapeutic relationship.
If a parent is hesitant, and I can reassure them by explaining that we can safely defer the non-urgent HepB dose to 6 weeks (per the NZ model) while ensuring they get the crucial Vitamin K injection at birth and commit to the full schedule from 6 weeks on, that is a massive clinical win. It keeps the family onboard and ensures their baby gets fully vaccinated
This is not "anti-vax." This is patient-centred, evidence-based paediatric practice.
Where the Conversation Broke Down
On social media, this nuance was impossible. My attempt to explain the rationale behind different national schedules was met with accusations of "dodging the question." The discussion wasn't a dialogue; it was a purity test.
The page administrators were not interested in why a clinician might tailor an approach to a specific family. They were interested only in policing a single, universal public health message. For them, any deviation from the script was heresy.
This highlights the core problem:
A Clinician's Goal: To apply broad evidence to a specific, unique individual, building trust to achieve the best possible outcome for that patient.
An Online Page's Goal: To broadcast a simplified, absolute message to a mass audience, often for engagement and brand identity.
When my expert, real-world perspective challenged their rigid brand, the simplest solution was not to engage with the data, but to remove me from the conversation.
The Trap of Scientism
This dynamic—where data is wielded as a weapon and context is dismissed as weakness—has a name: Scientism.
Science is a powerful method for understanding the material world. Scientism, however, is an ideology. It’s the excessive belief that the methods of natural science are the only source of genuine knowledge, and that they can and should be applied to solve all problems. It treats science not as a tool, but as a complete worldview that renders other forms of human knowledge, like clinical judgment, ethics, and experiential wisdom, irrelevant.
The response from the page was a textbook case of scientism. By treating the vaccine schedule as an unassailable text and framing any deviation as a moral and intellectual failure, they were defending an ideology, not the practice of science. Real science is about curiosity, debate, and updating our understanding. Scientism is about dogmatic adherence and shutting down dissent. It turns the quest for knowledge into an ideological purity test, where anyone who raises a valid question that complicates the simple narrative is labelled "anti-science."
This approach is not only unhelpful; it’s counterproductive. If our shared goal is to foster public trust and protect community health, scientism is a failing strategy. A better path involves:
Leading with Humility: Acknowledging the limits of our knowledge and being transparent about the trade-offs involved in any medical decision.
Valuing Dialogue over Proclamation: Treating questions from concerned parents not as attacks to be deflected, but as invitations to a conversation.
Building Trust, Not Demanding It: Earning trust by demonstrating respect, empathy, and a commitment to the individual patient’s well-being, not just by citing population-level data.
The Mission of This Space
I’m not outraged about being blocked. I’m motivated.
It's clear that we need a better forum. This Substack will be that forum. My goal is to pull back the curtain on the art and science of medicine. We will talk about:
The evidence behind recommendations and where the data is less clear.
How doctors navigate uncertainty and work with families to make shared decisions.
The gap between public health policy and individual patient care.
How to be a critical, informed consumer of health information without falling into the trap of misinformation.
This is a space for nuance. It’s a space for good-faith questions and thoughtful answers. It’s a space built on the trust that should be at the heart of all healthcare.
Thank you for being here at the beginning, let’s keep the conversation going and show the way forward to rebuilding trust in medicine.
Stay Informed, Not Overwhelmed.
Dr. Matt
Disclaimer: This information is for general educational purposes only and is accurate at the time of publication. It does not constitute medical advice, is not intended to be a substitute for professional medical advice, and does not establish a doctor-patient relationship. Always seek the advice of a qualified health professional for any medical concerns.
References & Further Reading
Here is a list of sources that inform the clinical points made in this post. I encourage you to read them to understand the evidence for yourself.
Australian Hepatitis B Vaccination Schedule:
Source: The Australian Immunisation Handbook, Department of Health and Aged Care.
Relevance: This is the official guideline for Australian clinicians. It explicitly recommends a universal monovalent dose of the Hepatitis B vaccine at birth for all infants.
Source: Australian Government, Department of Health and Aged Care.
Relevance: This is the official guideline and visual schedule for the Australian National Immunisation Program. It confirms the recommendation for a universal monovalent dose of the Hepatitis B vaccine at birth for all infants, providing a clear point of comparison with the New Zealand schedule.
New Zealand Hepatitis B Vaccination Schedule:
Source: The Immunisation Handbook, Ministry of Health | Manatū Hauora, New Zealand.
Relevance: This official NZ guideline outlines their risk-stratified approach, recommending the birth dose only for babies born to mothers with Hepatitis B, with the routine schedule for all other infants starting at 6 weeks. This directly supports the point that different, valid schedules exist in developed countries.
Source: The Immunisation Advisory Centre (IMAC), New Zealand.
Relevance: This page provides the official visual and text-based immunisation schedule for New Zealand, showing their risk-stratified approach which targets the Hepatitis B birth dose for high-risk infants and begins the routine schedule at 6 weeks for others.
Effectiveness and Importance of Antenatal Screening:
Source: Communicable Diseases Network Australia (CDNA).
Link: Hepatitis B - National Guidelines for Public Health Units
Relevance: These national guidelines detail the critical role of antenatal screening for Hepatitis B in preventing perinatal transmission and identifying the risk status of newborns, which is the foundation of the targeted approach.
Long-Term Immunity (Birth Dose vs. 6-Week Start):
Source: Schillie, S. et al. (2018). "Prevention of Hepatitis B Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization Practices." MMWR Recomm Rep, 67(1), 1–31.
Relevance: While a US document, this comprehensive review provides data on vaccine efficacy. It notes that "seroprotection rates are similar" for infants of HBsAg-negative mothers who begin the series at birth versus those who begin several weeks later, supporting the clinical argument about similar long-term outcomes.
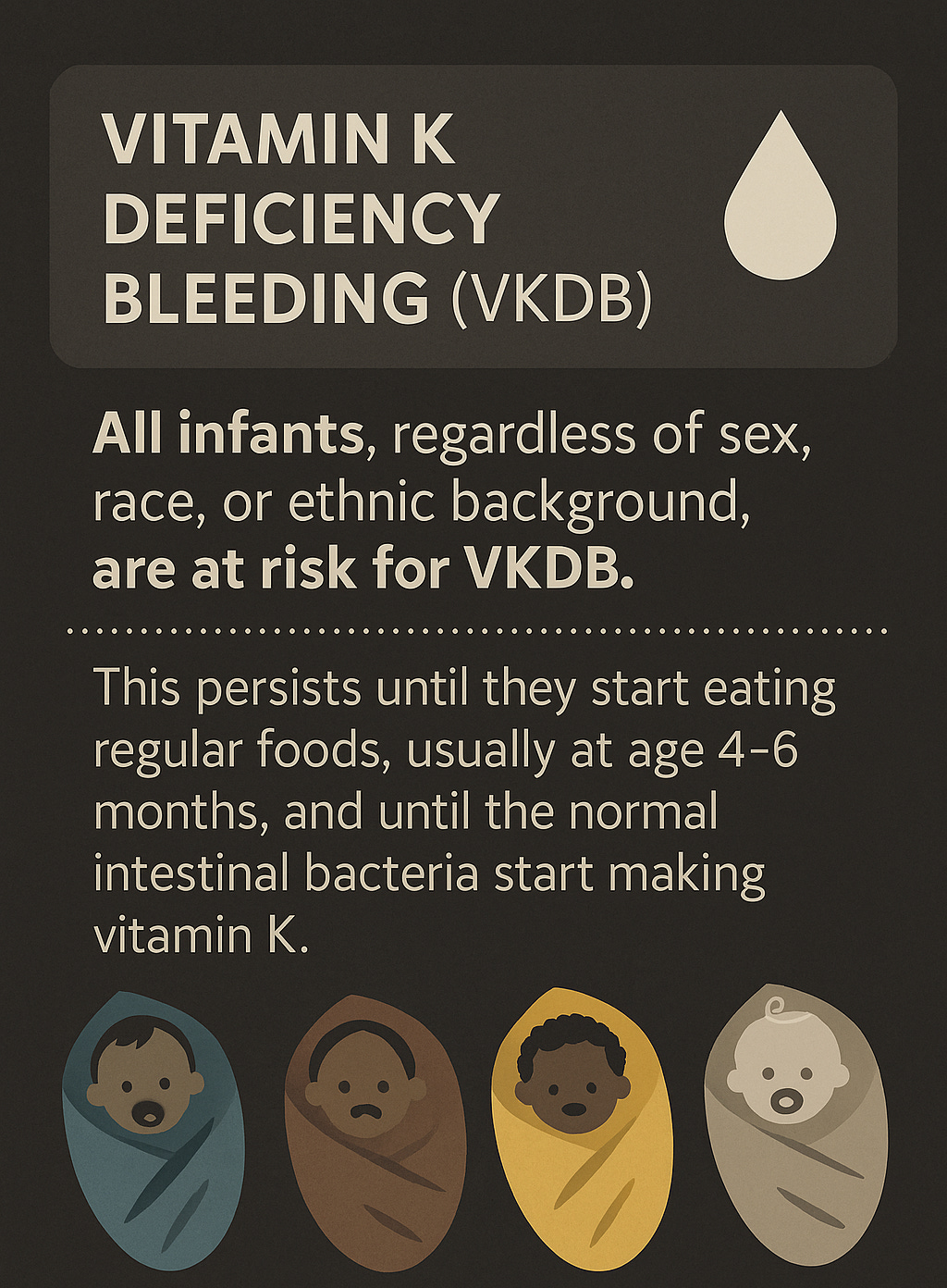
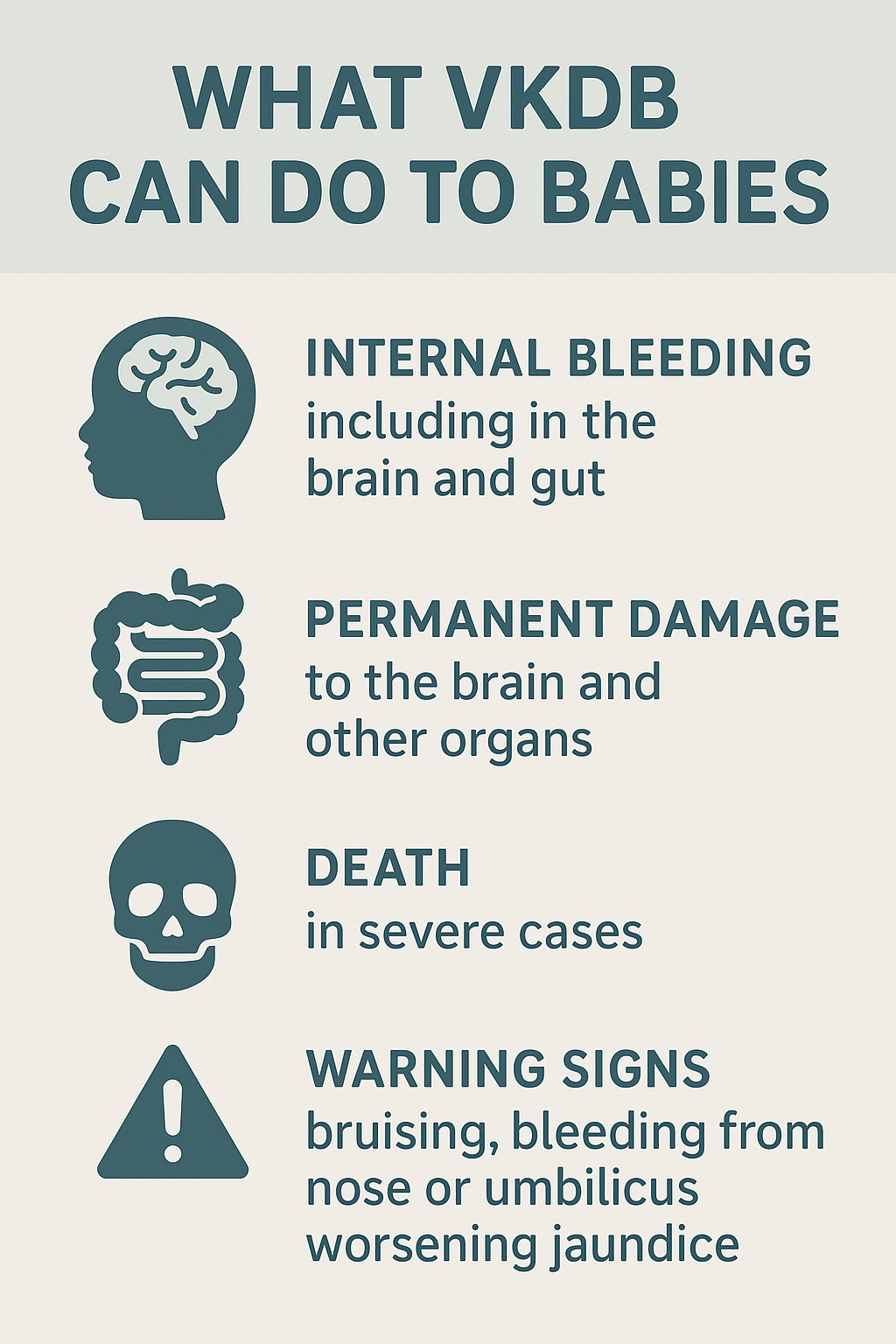
The Critical Importance of Vitamin K:
Source: National Health and Medical Research Council (NHMRC).
Link: Joint statement and recommendations on vitamin K for newborns
Relevance: This is the key Australian authoritative document confirming the vital role of Vitamin K administration at birth to prevent Vitamin K Deficiency Bleeding (VKDB), reinforcing why it's a non-negotiable intervention compared to the more flexible timing of the HepB vaccine in low-risk babies.
Shared Decision-Making in Clinical Practice:
Source: Australian Commission on Safety and Quality in Health Care.
Relevance: This resource from Australia's lead agency for safety and quality in healthcare defines and promotes shared decision-making as a cornerstone of patient-centred care, validating the collaborative approach with parents described in the post.







Hey Matt, pretty interesting stuff here. As someone without medical training, I find it alarming that even having attempting to engage in discourse about this topic on social forums gets censored. Why does there need to be a media intermediary preventing open discussion? I hope that we can get to a place as a society where we can ask questions, or present ideas. Looking forward to reading more